The Patient's Journey: PCORI's Investment in Research across the Cancer Continuum
An estimated 1.6 million people are diagnosed with cancer every year in the United States. With an aging population, the number of patients with cancer is projected to increase significantly over the coming years. Patients, caregivers, and their care teams need evidence-based information on prevention, diagnosis, treatment, survivorship, and palliative care options to make critical decisions that significantly impact patient outcomes.
PCORI has invested in comparative clinical effectiveness research (CER) to inform some of the most pressing issues facing cancer care today, including how to best address known cancer disparities in morbidity and mortality, support difficult preference-sensitive treatment choices that require significant trade-offs, facilitate post-treatment survivorship care planning, and expand access to comprehensive palliative care services for patients living with advanced cancer and their caregivers.
This blog provides a brief overview of PCORI’s overall cancer portfolio and describes some of the individual research investments made to address many of these critical issues across the patient’s cancer journey.
Portfolio Overview
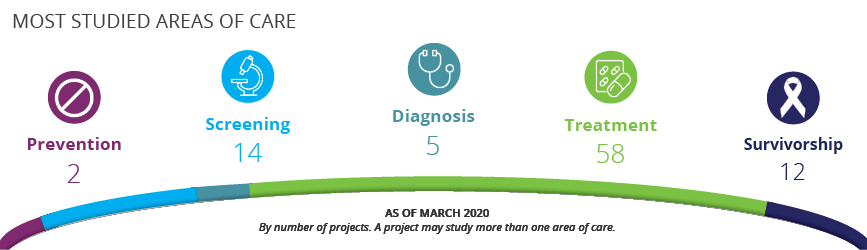
PCORI funds patient-centered outcomes research (PCOR), a type of CER that focuses on questions and outcomes that matter to patients and the people who care for them. To date, PCORI has funded more than 80 CER studies on cancer. Our cancer portfolio reflects this patient-centered focus, with many of the studies evaluating clinical and patient-reported outcomes in real-world settings.
Our studies also often include patient populations traditionally excluded from cancer clinical trials, such as older adults and those with comorbid health conditions. PCORI cancer studies are evaluating the comparative effectiveness of a range of clinical, communication, and care delivery interventions, with about 70 percent of the studies designed as randomized clinical trials with more than half of the trials having large patient samples of more than 500—a size that supports subgroup analyses.
PCORI requires funded investigators to engage stakeholders throughout the research project to ensure the research questions and findings are relevant to patients and the people who care for them. Patients and other stakeholder partners work closely with research investigators on PCORI-funded cancer studies to help guide and inform design, outcomes measured, and dissemination strategies. One area emphasized by stakeholders that has been missing to date in research is the assessment of caregiver outcomes. Over one-quarter of our cancer studies also enroll family caregivers who face a significant burden in caring for cancer patients.
We believe the conduct of PCORI-funded PCOR, a sampling of which we explore below, will produce useful results for cancer patients and those who care for them across their cancer journey.
PCOR Across the Patient Journey: Addressing Disparities in Prevention and Early Detection
Addressing disparities is one of PCORI’s five national priorities for research, and an important focus in the cancer portfolio. Cancer health disparities among racial and ethnic minorities and the socioeconomically disadvantaged suggest that effective prevention and early detection strategies do not reach all Americans. PCORI has funded several studies that address barriers to uptake of evidence-based interventions in populations at risk for cancer disparities.
One study, led by Ronald Myers, PhD, at Thomas Jefferson University, addresses known disparities in colorectal cancer screening. Hispanics and Latinos have considerably lower colorectal cancer screening rates than the national average, which contributes to a greater burden of advanced colorectal cancer at diagnosis and death from colorectal cancer than other populations.
Myers’ team evaluated two proven methods of active decision support to identify the most effective approach for increasing uptake of colorectal cancer screening among Hispanic patients. The results showed that personalized phone calls providing informational and navigation support lead to a greater proportion of patients completing colorectal cancer screening at one year, 78 percent, than those who received mailed bilingual materials alone, 44 percent. These results can help clinicians and health systems learn best practices for improving uptake and reducing known disparities in screening.
Another ongoing PCORI-funded study by Roshan Bastani, PhD, at the UCLA School of Public Health aims to reduce health disparities in Los Angeles County, where underserved Hispanic patients are disproportionately impacted by human papillomavirus (HPV)-related cancers. HPV is a sexually transmitted infection that can lead to cancer, but a vaccination for youth and young adults can protect them from infection. This study is comparing three parent- and provider-level strategies to increase the number of boys and girls who get the HPV vaccine. Parents are one of the direct recipients of this study’s intervention, which underscores the importance of caregivers and their influence on patient health outcomes.
Preference-Sensitive Treatment Options
Studies comparing treatment options make up the largest portion of our cancer portfolio. These studies aim to provide a more complete picture of risks and benefits of treatment options so that patients can make choices that align with their preferences. Patient-centered information is especially significant for cancers where important trade-offs are considered with no clear-cut course of action.
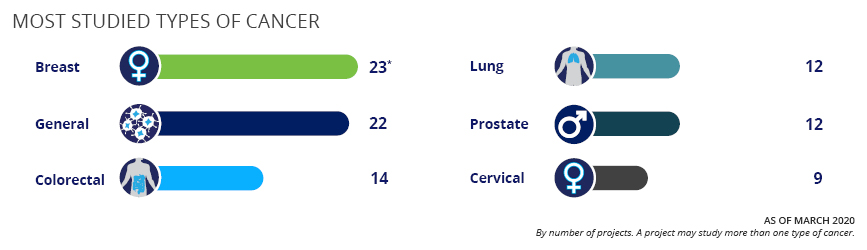
Treatment for localized prostate cancer is a preference-sensitive choice. A study led by David Penson, MD, MPH, at Vanderbilt University compared three contemporary approaches to managing localized prostate cancer—active monitoring, radiation, and surgery—among a racially diverse group of men. The team found surgery was associated with long-term urinary incontinence and sexual dysfunction compared to radiation or active monitoring, while no difference among the procedures was observed in bowel symptoms or quality of life beyond the first year of treatment. These results add to a growing body of evidence on important trade-offs between the clinical and patient-reported outcomes men with clinically localized prostate cancer need to consider when making treatment decisions. The study team has also received a related PCORI Dissemination and Implementation Award to implement a decision aid in health systems in Tennessee and California using updated data from the PCORI-funded prostate cancer study.
Another ongoing PCORI-funded study led by John Gore, MD, MS, at the University of Washington evaluates preference-sensitive choices related to bladder cancer recurrence on overall patient quality of life. Patients can choose between surgery that removes the bladder and medication. Surgery usually cures the cancer, but patients report an impact on sexual function and decrease in quality of life. Medical management allows patients to keep their bladders and avoid the side effects of surgery, but it may not be as effective as surgery in curing cancer. In addition to patient quality of life, caregiver burden is being evaluated as a key outcome demonstrating the need for more evidence on the caregiver experience so that it may be considered during preference-sensitive treatment decisions. This research study was preceded by a Eugene Washington PCORI Engagement Award that identified questions and outcomes prioritized by patients and caregivers.
Survivorship Care Planning and Post-Treatment Surveillance
Patients who have finished cancer treatment need a survivorship care plan—a roadmap for follow-up care that considers a patient’s prior treatment. Since 2015, the Commission on Cancer, a consortium of professional organizations dedicated to improving survival and quality of life for cancer patients, has required cancer centers, as a condition of accreditation, to provide their patients with survivorship care plans at the end of their treatment. However, questions remain about what models of survivorship care plan delivery work best for ensuring adherence to the recommended follow-up care. A PCORI-funded study led by Katherine Smith, PhD, at Johns Hopkins University, aims to fill this evidence gap by comparing three different approaches to delivering survivorship care plans following treatment. Study results will inform oncology providers on the extent of communication needed with patients to ensure adherence to recommendations included in the survivorship care plan.
This PCORI-funded researcher and clinician shares some of the most common benefits and drawbacks of cancer surveillance, including patient anxiety.
One component of the survivorship plan is frequency with which the patient should undergo post-treatment surveillance. Although guidelines recommend continued surveillance, for many cancer sites, the optimal frequency and timing of post-treatment surveillance is somewhat uncertain. PCORI has funded several projects comparing more versus less frequent surveillance strategies for some of the most commonly treated cancers, including colorectal and lung cancer. Both studies reported little difference in clinical outcomes, including cancer recurrence and overall mortality, between the more versus less frequent post-treatment surveillance approaches. These results contribute to a growing body of evidence that suggests for some cancer patients, less frequent post-treatment surveillance is a viable option and may not compromise long-term clinical outcomes.
Access to Advanced Cancer Care
While the number of cancer survivors in the United States has been rising significantly, patients unfortunately sometimes face a cancer with no curative treatments. Patients, caregivers, and care teams in this situation still face questions about how to minimize symptoms and optimize support and comfort.
Palliative care focuses on improving patient and caregiver quality of life by providing relief from treatment side effects, addressing symptoms such as pain or anxiety, and by reducing caregiver burden. Palliative care also helps facilitate discussions between patients and their families so that care at the end of life is consistent with their goals and preferences. But many hospitals and clinics don’t have qualified staff to provide this type of care for all patients, and patients in areas underserved by health professionals might not have access to palliative care at all.
To address this lack of accessibility, an ongoing PCORI-funded study led by Jennifer Temel, MD, and Joseph Greer, PhD, at Massachusetts General Hospital is examining, in several cancer centers across the country, whether palliative care sessions delivered via videoconference could be an effective alternative to in-person visits. Over a period of five years, the researchers will compare the two groups for a range of patient-centered and caregiver outcomes. If it’s found to be effective, palliative care delivered via telehealth modalities such as videoconference could dramatically increase access to high-quality care for patients living with advanced cancer and their caregivers. This study is one of several CER studies PCORI has funded that address the needs of patients with advanced illnesses.
In the coming months, stay tuned for additional blogs that take a more detailed look at PCORI’s research investments on several specific cancer types, and how the research is addressing relevant issues across the patient journey.
Cancer Research in Context of COVID-19
This overview of PCORI’s cancer portfolio shares examples of how PCORI-funded studies are addressing critical evidence gaps across the patient’s cancer journey. New decisional dilemmas are likely to emerge and be amplified in the current context of the COVID-19 pandemic. While publications are limited, mounting evidence suggests that adult patients with cancer, especially patients undergoing active treatment, are at higher risk of developing COVID-19, experiencing a more severe course, and dying at higher rates from COVID-19 than the general population.
During the pandemic, patients with cancer are also likely to experience delays in much-needed cancer treatments. Healthcare providers and cancer centers are faced with the challenge of how best to minimize exposure among cancer patients requiring treatment and monitoring during the pandemic without significantly delaying their treatments. To address the needs of vulnerable individuals including cancer patients and survivors, the PCORI Board of Governors has approved dedicated funding to support research on COVID-19 that will inform critical decisions on how best to optimize care for these patients during the pandemic.